
The school’s global health efforts focus on sustainable, capacity-building efforts. In the DRC, reproductive health research employs many locals.
The Celia Scott Weatherhead School of Public Health and Tropical Medicine has been committed to global health since its founding in 1912. For fifteen years, the school’s tag line was: a global commitment to public health.
That leadership has saved lives.
The field of global health, however, is undergoing dramatic change as the United States closed the U.S. Agency for International Development (USAID) earlier this year, ending many longstanding programs, and has instituted several other drastic cuts in other agencies and departments that also touch public health.
The changes have left many researchers wondering, what’s next? Many have dedicated their entire professional lives to global public health. We caught up with several researchers to find out how they are moving forward amidst disruption.
Malaria Reduction
Malaria is spread by a simple mosquito bite, yet it has been a leading cause of child mortality for decades—despite being completely treatable.
In the late 1960s, financial, political, and technical challenges, including insecticide and drug resistance, led to major funding cuts to malaria programs in many endemic countries. That stagnation spurred a resurgence of malaria across the world.
By the early 2000s, up to one half of all child deaths in endemic areas of Africa were attributable to malaria. But new tools such as insecticide-treated nets, artemisinin-based combination therapies, and rapid diagnostic tests were becoming available. In 2002, the Global Fund was established to combat malaria, HIV, and tuberculosis.
The momentum in malaria control convinced George W. Bush to establish the US President’s Malaria Initiative (PMI) in 2005, and since then, investments in malaria control have saved millions of lives.
Tulane’s longstanding reputation within the field of tropical medicine made it a natural partner for malaria research. Dr. Don Krogstad, former chair of the Department of Tropical Medicine, began conducting research and training in Mali, West Africa, and in 2010 established the NIH-funded International Center of Excellence in Malaria Research.
A few years later, that effort was joined by the Tulane Center for Applied Malaria Research and Evaluation (CAMRE) and since then interdisciplinary research at Tulane has resulted in over 150 peer-reviewed publications, with findings that have influenced both national and global malaria policies and programs.
Their work has included estimating the effectiveness of malaria prevention interventions through systematic reviews and meta-analyses, evaluations of new interventions using rigorous randomized trials, impact evaluations of national malaria control programs, geostatistical analysis and risk mapping, translational research on increasing the uptake and use of insecticide-treated mosquito nets (ITNS), and measuring malaria parasite prevalence using population-based household surveys.
Dr. Thomas Eisele, CAMRE director, points to the center’s research as key to the battle against malaria.
“We've been contributing to the evidence base for essentially 25 years now, and I think that's really where we've made the most impact in malaria control, in evidence of how well things are working and new interventions,” he said.
The group has established a solid track record in research funding, with over $6 million in funding from the Gates Foundation, the National Institutes of Health, the Centers for Disease Control and Prevention, USAID, and the World Bank, in countries including Zambia, Ethiopia, Benin, Ghana, Mali, Malawi, Tanzania, Senegal, the Gambia, and Eritrea.
A recent project funded by the Gates Foundation involved large-scale community randomized control trials with targeted sugar baits, a novel vector control tool.
“We've been really at the forefront of evaluating the impact of new malaria control and elimination tools,” says Eisele
According to a 2015 paper in Nature co-authored by Eisele and Dr. Josh Yukich of CAMRE, incidence of clinical malaria fell by 40 percent between 2000 and 2015. Interventions have averted an estimated 663 million clinical cases since 2000.
PMI’s funding could see a reduction by as much as 50 percent for fiscal year 2026. A recent paper by the Malaria Atlas Project in The Lancet estimates that Africa could expect to see an additional 13.6 million cases and an additional 104,000 deaths due to malaria in a single calendar year, all due to funding loss.
Eisele stresses that the work is important not only because of the human impact at the global level, but also for economic and national interests too.
“Malaria was endemic in the United States until the 1950s, so that's one of the original missions of the CDC, the wish to combat malaria,” Eisele points out, noting that the vector that spreads malaria is still here, people can bring the parasite that causes malaria to the U.S. through travel, and the climate in the South is very suitable for spread.

Good surveillance is critical for keeping the numbers in the United States lower. But there’s also a negative economic impact to letting the disease rage unabated across the globe. Curbing any sort of investment abroad represents a wasted opportunity for building economic collaborations that go beyond malaria.
“It's really a matter of will, because it is a completely preventable and treatable disease,” Eisele says. “No kid should ever die of this. We have treatment. It's not a chronic disease, it's not something we can't cure. It is cured with a course pill that you take over three days.”
With an eye on saving malaria prevention, Eisele is convening with faculty across the school to help map out a strategy for the school as it navigates a different funding landscape.
“It won't look the same as it does now, but how can we help position the school and university to be competitive in that new environment. There's a number of us that work in global health that are trying to think about this and be proactive.”
Building Capacity
A frequent topic in global health these days is “decolonizing” the field. Dr. Ron Blanton, chair of Tropical Medicine and Infectious Disease, often talks about the history of tropical medicine, which was rooted in benefits for the colonizing country.
As a long-time advocate in the field, the Celia Scott Weatherhead School has taken an active role in ensuring that researchers aren’t conducting research on a country, but with that country and the citizens of the region. The school’s focus has been on building capacity in country and ensuring that efforts are sustainable.
One outcome of this approach has been the launch of training programs to help low-income countries develop the personnel to address public health concerns independently.
In several instances, that training has gone a step further, with the school taking an active role in helping to establish new schools of public health in low-income countries. Dr. Bill Bertrand, professor emeritus of IHSD, was instrumental in establishing the first such school: the Kinshasa School of Public Health in the Democratic Republic of Congo. Other schools and programs have been launched in Ethiopia, Rwanda, Senegal, Vietnam, and Uganda.
Dr. Nancy Mock, an international development expert with nearly 40 years of professional experience in more than 30 countries, likened Tulane’s role with these schools—dating back to the 1980s—as akin to being a “leadership machine.”
“That's enormously high impact, and it’s sustainable,” she explains. “You begin to train people in these countries at these schools. And every year, you're pumping out however many [students]...who go out into the health zones and help lead public health efforts.”
Tulane’s involvement has not been limited to faculty training and teaching.
“We looked at the whole institution,” Mock says. “Do they have the ability to manage grants? Do they have financial management capacity? Do they have leadership, training and staff? So, we looked at it more from an institutional development perspective.”
Mock notes that funding for these efforts often comes from local governments, and additional donor funding may be more enthusiastically offered for programs proven to be self-sustaining.
Each of the schools Tulane has assisted is doing well. “They're doing research, they're partnering in intelligent ways, and they’re training the leaders of their country in the health sector. That's the highest impact work Tulane has done, really.”
The impact also does not flow in just one direction, says Mock. Experiences in low-income countries often resemble health concerns here, particularly in rural communities. “The work we do internationally is extremely relevant to that. I think we can do really transformative work here in the U.S. based on our global work.”
In addition to helping to establish independent schools of public health around the world, Tulane’s Weatherhead School has leaned into the concept of helping individual communities find healthcare independence in several other ways.
The school’s participation in Data for Impact, an extension of the MEASURE Evaluation project, assisted low- and middle-income countries in increasing their capacity to use available data and generate new data to build evidence for improving health programs, health policies, and decision making. The program provided more than 300 individual assessments of data to more than 30 participating stakeholders to assist in program decision-making.
International food security has been another way Tulane has leaned into capacity building. Bertrand and Mock worked together in the 1980s to develop a famine early warning system.
“For a long time, we actually got pretty good at avoiding catastrophic famine or high mortality from people starving to death,” Mock says. That experience is becoming more relevant today as famines are once again becoming more prevalent. She worries that pandemics and other large-scale health emergencies are also more likely. She’s heartened, however, by Tulane’s experience combatting those issues. “There are all these people out there and institutions who we've partnered with and played a role in their development, and [they have] some of the answers to these problems.”
Mock sums up the kind of work Tulane researchers do: “We're trying to enable them to manage [risks] themselves, as opposed to relying on humanitarian assistance from the United States.”
Through the Alumni Lens: The State of Public Health
CHARLES N. “CHIP” KAHN III (PHTM ’80)
“Public health today faces serious disruption: rising disparities, shaky institutional foundations, and policy changes that threaten health coverage expansion—which has long been a core professional goal of mine. Over many decades, I’ve held fast to the idea that health coverage is essential; without it, prevention fails, access is uneven, outcomes suffer. Since the start of the year, the Trump Administration and HHS Secretary Robert F. Kennedy Jr. have pursued sweeping changes: massive staff cuts at HHS, the retooling of agencies under the “Administration for a Healthy America” agenda and ambitious restructuring that critics say will weaken the federal public health infrastructure. Meanwhile, the One Big Beautiful Bill (OBBBA), now law, includes large cuts to Medicaid and tighter eligibility rules—moves that risk rolling back coverage gains. My perspective remains consistent: public health must be equitable, preventive, and anchored in universal coverage. What’s evolved is a sharper urgency: institutional disruptions don’t just inconvenience agencies—they endanger real lives by undermining both access and trust.”
DR. GREG BUCHERT (PHTM ’79, M ’83, R ’85)
“I am disappointed in the current state of public health. Between increasing mistrust of authority, lack of independent thinking elected officials and an increasing skepticism of the best science we know, it does not bode well for public health. For decades, I’ve been disappointed by the low profile of public health and the lack of awareness of its importance in our lives. Now that it is thrust in the limelight during this current environment, I long for those low-profile days of effective, accepted science-based interventions.”
CHRISTOPHER RICHARDSON (TC ’99)
“Public health may be more important to humanity than it has been since the aftermath of WWII, but it is facing perhaps the greatest threats and challenges, from multiple fronts, in recent memory. In light of increased politicization, rising skepticism, a break-down of global collaboration and outright unscientific groupthink and conspiracy theories, we are facing a crisis that only strong and dedicated institutions like the WSPH can seek to address.”
“Right now, trust in public health entities is being eroded. My views of the necessity for public health systems has not changed over the years.”

Family Planning

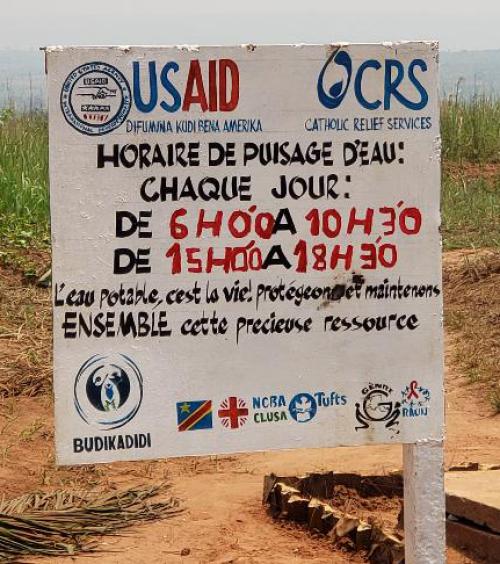
Tulane’s faculty have worked in family planning in multiple countries worldwide, but none more extensively than the Democratic Republic of Congo (DRC, formerly Zaire). In the 1980s, Jane Bertrand led several pioneering projects in community-based contraception and helped to create an evaluation unit for the national family planning program. After a 20-year hiatus resulting from political turmoil in the country, the Gates Foundation and subsequently the Packard Foundation approached Tulane to continue its work in family planning in the DRC.
“Tulane had this real advantage that we understood the country, felt comfortable working there, and had established colleagues within the public health community,” Bertrand says. “The work that started in the 1980s made Tulane attractive to donors as a potential grantee and enhanced its ability to restart its family planning programming in the 2000s.”
In the 1990s, Tulane was one of the original partners on the MEASURE Evaluation Project, which initially focused on family planning. Dr. Mai Do, Dr. Katherine Andrinopoulos, Dr. Janna Wisniewski, and Dr. Marta Silva, all faculty in international health and sustainable development, were among those leading family planning activities under these projects.
During the decade of the 2010s, Tulane’s family planning work in the DRC accelerated with funding from multiple donors, and Dr. Julie Hernandez and Dr. Anastasia Gage added their expertise to this growing operation. Tulane established a local office in Kinshasa under the banner of Tulane International, which became Tulane’s largest overseas office, and is currently overseen by Country Director Dr. Arsene Binanga with 15 Congolese staff.

Since then, Bertrand has served as principle investigator on grants totaling more than $60 million, and since 2017 Hernandez has added $23 million to that total. “Tulane was in the right place at the right when donors were eager to invest in family planning in the DRC,” says Bertrand.
As Tulane’s portfolio of family planning projects increased, the Center for Reproductive Policy and Programs was established in 2018 to manage this work, with Bertrand as director and Maria Herdoiza serving as associate director. With Bertrand’s retirement, Hernandez has taken on the director role.
As funding for international development was severely impacted by the dismantling of USAID in early 2025, Tulane has continued to advance family planning in the DRC through support from other donors. In June 2025, Tulane was awarded $18 million from the Central African Forest Initiative for phase 2 of its PROMIS project.
In many low- and middle-income countries, family planning has been among the most cost-effective interventions in public health. In the DRC, it remains a challenge, due to multiple factors: grinding poverty, the low status of women, misinformation and myths about contraception, and religious beliefs, among others. Yet Tulane in collaboration with the DRC Ministry of Health and other NGOs continues to work toward increasing access to family planning for women and girls in this country.
Into the Future
The Celia Scott Weatherhead School of Public Health and Tropical Medicine’s impact on the global stage extends well beyond the programs mentioned here. The diversity of research and programming is impressive in its own right, but it’s the school’s ability to adapt and identify key focus areas that ensures the school will continue to lead on the forefront of global health.
“We've always said we're trying to work ourselves out of a job,” said Bertrand. To some degree with the loss of USAID, that is currently the case. However, the school also has helped establish a legacy of well-trained professionals who are positioned to continue to make an impact.
“Building capacity is a watchword within international development,” Bertrand adds. “And I think that our operation has done an excellent job in that area.”

